If you're a Medicare beneficiary, you know that having access to affordable medications is critical for maintaining your health and wellbeing. Medicare Part D is part of the federal program that helps coordinate your prescription drug coverage that you've purchased through a private insurance company, but it's not always easy to understand which medications are covered and which are not.
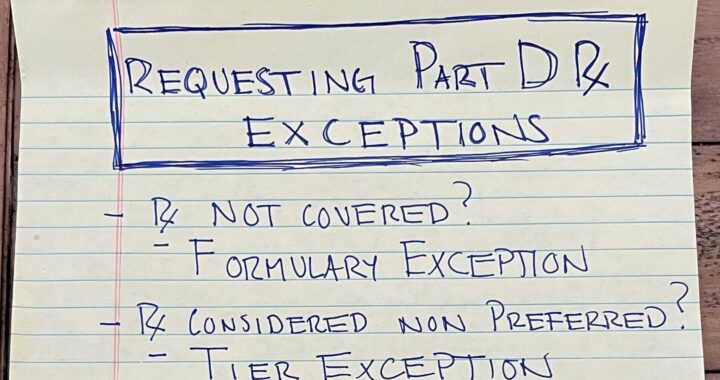
One issue that many Medicare beneficiaries face is coverage limitations for certain medications. These limitations can include Tier Exceptions, Formulary Exceptions, and restrictions on Step Therapy, Quantity Limits, and Dosage Limits. Fortunately, there are ways to request exceptions to these limitations and ensure that you have access to the medications you need.
Tier Exceptions: Medicare Part D drug plans often have different "tiers" of coverage, which determine how much you pay for each medication. If your medication is not on the preferred tier, you may have to pay a higher cost-sharing amount. However, you can request a Tier Exception to get a lower cost-sharing amount for a specific medication.
Formulary Exceptions: The formulary is the list of medications that your Medicare Part D plan covers. If your medication is not on the formulary, you may have to pay the full cost of the medication. However, you can request a Formulary Exception to get coverage for a specific medication that is not on the formulary.
Medicare Part D plans may also have restrictions on Step Therapy, Quantity Limits, and Dosage Limits. Step Therapy requires you to try less expensive medications before trying more expensive ones, while Quantity Limits and Dosage Limits limit the amount of medication you can receive. However, you can request exceptions to these limitations if you and your doctor believe that they are not appropriate for your health needs.
To request exceptions to these coverage limitations, you or your doctor can submit a form to your Medicare Part D plan. You'll need to provide information about your medical condition and why the requested exception is necessary. Your Medicare Part D plan will review your request and let you know if it has been approved or denied within 72 hours.
Don't let coverage limitations for your medications hold you back from living your best life. Explore your Medicare Part D benefits and talk to your doctor about whether exceptions may be appropriate for you.